The Maternal Vulnerability Index can be used to support a precision response to postpartum depression
Postpartum depression (PPD) is the most common complication post-childbearing, affecting 1 in 8 mothers nationally. It’s not simply “baby blues”, it’s a more severe form of sadness and tiredness that comes after giving birth, a time that already can be incredibly stressful and challenging. Disturbingly, less than half of all mothers affected are diagnosed, and only about 2 in 10 mothers with PPD are treated. What’s more, Black and Latina mothers were about half as likely as white mothers to initiate treatment.
The first step to treatment is ensuring that women are universally screened for postpartum depression during their postpartum visits
Unfortunately, our new analysis shows as many as 1 in 4 women report not getting screened for PPD. Our data shows that 5% to 13% of mothers across states do not attend a single postpartum visit, which aligns with other studies of postpartum visit prevalence. What’s more, of women who do receive postpartum care, our analysis shows that an average of 14% report not being screened for postpartum depression.
Our analysis suggests postpartum depression screening gaps occur across the US with some states more than others — for example, Nevada has a 28% screening gap as compared to Oregon that only has a screening gap of 4% (Figure 1). Screening gaps are more acute for women of color; one study from a large health system in Minnesota found that compared to White women, Black women were 36% less likely to be screened, and Native American, Hawaiian, Alaska Native and multiracial women were 56% less likely. Though health policy choices such as Medicaid expansion are sometimes correlated to the political affiliation of the state, the 10 states with the largest gaps are a mix of traditionally Republican and Democrat-leaning states.
The MVI can be used to help identify communities vulnerable for postpartum depression and to explore the reasons why
Surgo’s Maternal Vulnerability Index is a county-level, national-scale, open source tool that can be used to support postpartum depression reduction strategies. The MVI is designed to support policy makers and community based organizations identify where and why women are vulnerable for poor maternal health outcomes such as maternal mortality and preterm birth with precision. The MVI can also be extended to support postpartum depression.
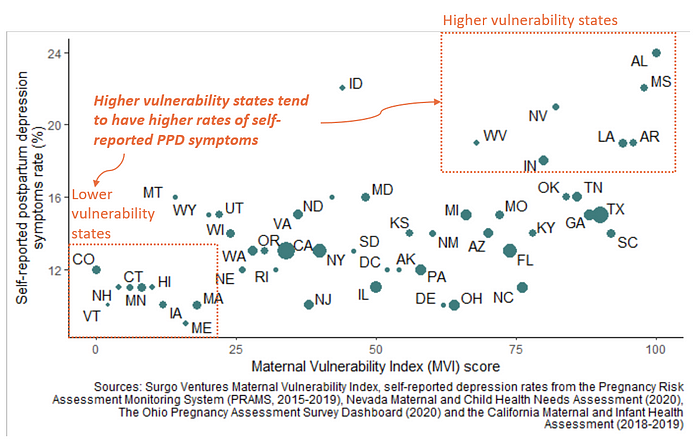
Our analysis shows that mothers living in higher vulnerability states, as defined by the MVI, were 1.3 times more likely to have self-reported postpartum depression symptoms (Figure 2). This shows that practitioners, policy makers, and researchers can use the MVI to identify specific areas that are likely to have a higher burden of PPD; they can identify the states and counties with higher MVI scores and plan their resourcing, interventions, and policies accordingly.
In addition, many of the risk factors for postpartum depression and barriers to access care are also indicators that are incorporated into the vulnerability themes within the MVI. For instance, food insecurity is a risk factor for PPD, which is incorporated into the “socioeconomic determinants” MVI theme. Access to transportation, included in MVI theme “physical environment” may affect the ability to access mental health treatment. Figure 3 highlights each of the six MVI themes and the types of indicators each theme incorporates.
Given this, practitioners and researchers can use the MVI to zoom in on the individual themes that are scoring the highest for a given county to better understand the types of risk factors that might be driving postpartum depression in that geography. They can also use it to explore the interventions that may be needed in that area — informed by the area’s highest scoring themes and risk factors.
Figure 4 provides an example of how this could work. In this case, Brooklyn, NY, has a few high scoring themes in the MVI. Priority risk factors and corresponding interventions can be considered that are focused on these themes. Since “physical environment” is the theme with the greatest vulnerability, one might consider subsidized access to transportation as one possible intervention. The MVI is a tool that should complement local understanding and public health expertise to make decisions with precision.
Additional policies and data are still needed to reduce postpartum depression
Many additional policies should also be put in place. One study in Oregon found that postpartum depression screening and treatment improved after Medicaid Expansion. However, expanding Medicaid coverage to one year postpartum has not been achieved in 6 states. States should also identify and scale promising models that link women to care — studies show interventions such as nurse home visitation and training providers on actively engaging patients can be effective. Paid parental and family leave can also help, which at present only nine states offer.
While gaps exist in postpartum depression screening, mandating the practice has some debate. There is a lack of evidence to prove that such screening laws increase the number of women in treatment. Even so, as of 2018, three states have required postpartum screening.
Addressing the challenge of postpartum depression and maternal vulnerability more generally requires a comprehensive approach. The MVI provides a starting point for policy makers and implementers to identify risk factors in specific geographies. We need more high quality data at the county level to further inform our response, including centralized access to county level data on postpartum depression, postpartum depression screening rates, and treatment rates.
